The Good, the Bad, the Ugly and Alternatives to Antibiotics
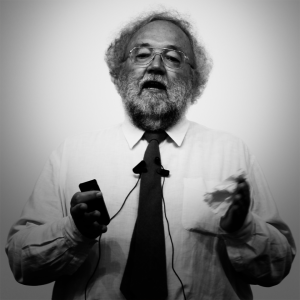
prof. Thomas V. Riley | University of Western Australia, Perth, Australia
medicina
| farmacija
This presentation suitable for general public will be about the consequences of inappropriate use of antimicrobial agents and some of the alternative approaches to treating infectious diseases that are being investigated like naturally occurring antimicrobials, such as honey and plant essential oils, probiotics and bacteriophage therapy. The emergence of multiple antibiotic resistant organisms in the general community is a serious threat to public health. Antibiotic resistance has finally prompted a revision of antibiotic utilisation, in part because the development of additional antibiotics has slowed. However, new antibiotics will not relieve the underlying selection pressure that drives the development of resistance. A paradigm shift in the treatment of infectious disease is necessary to prevent antibiotics becoming obsolete and, where appropriate, alternatives to antibiotics ought to be considered. There are already several non-antibiotic approaches to the treatment and prevention of infection including probiotics, bacteriophages and phytomedicines. Probiotics are live microbial supplements that are beneficial to the host. There is some evidence that probiotics such as Lactobacillus spp. or Saccharomyces boulardii are useful in the prevention and treatment of diarrhoea, including Clostridium difficile-associated diarrhoea that can be difficult to treat and recurs frequently. Bacteriophages are viruses active against bacteria and they have received renewed attention for the control of both staphylococcal and gastrointestinal infections. Phytomedicines, or plant-derived medicines, that have been utilised in the treatment of infections include artesunate for malaria, tea tree oil for skin infections, honey for wound infections and cranberry juice for urinary tract infections. Many infections may prove amenable to safe and effective treatment with non-antibiotics and patients are happy with these treatments. Governments need to fund appropriate research to support or refute the use of these agents for infectious diseases.
prof. Thomas V. Riley